All published articles of this journal are available on ScienceDirect.
Comparative Evaluation of Thyroid Nodule Malignancy Risk: FNA, Touch-Imprint Cytology, and Permanent Pathology
Abstract
Background
One of the most prevalent forms of solid tumors, especially in women, is thyroid cancer, and it affects more people worldwide than ever before.
Objectives
This study aimed to evaluate the accuracy of Fine Needle Aspiration (FNA) and touch-imprint cytology compared to permanent pathology, which is the gold standard in diagnosis.
Methods
This study was conducted as a retrospective cohort. According to the results of FNA and other supplementary tests, all the people who went to the Shahid Madani Medical Training Center in Karaj for a thyroid mass had indications for surgical removal of the thyroid mass and a definite diagnosis based on the final pathology.
Results
A total of 110 people were included in the study, and the average age of all patients included in the study was 46.34 years, with 74.26% of patients being female and 25.74% being male. According to results from permanent pathology, there were 39 cases of thyroid cancer, compared to the 28, 29, and 30 cases of cancer reported by Fine-needle Aspiration Biopsy (FNAB), touch imprint, and frozen section cytology, respectively. In the FNAB test, sensitivity was 69.2%, specificity was 98.4%, positive predictive value was 96.4%, negative predictive value was 83.6%, and accuracy was 87.12%. In the touch-imprint cytology test, sensitivity was 74.4%, specificity was 98.4%, positive predictive value was 96.7%, negative predictive value was 85.9%, and accuracy was 89.1%. In the frozen section cytology, sensitivity was 76.9%, specificity was 100%, positive predictive value was 100%, negative predictive value was 87.3%, and accuracy was 91.09%.
Conclusion
The results of this study show that ultrasound, frozen section cytology, FNAB, and touch imprint have high accuracy in diagnosing thyroid malignancies compared to permanent pathology, so they can be used as a reliable method for diagnosing thyroid malignancies to prevent the use of invasive and very expensive methods like surgery.
1. INTRODUCTION
Thyroid cancer is one of the most prevalent solid tumors, particularly among women, and its incidence has been steadily increasing worldwide [1]. Thyroid malignancies account for approximately 5–15% of all thyroid nodules, making accurate diagnosis and early detection critical for effective management and improved patient outcomes [2]. In some cases, small-sized papillary carcinomas can be managed non-invasively or through active surveillance, highlighting the importance of precise diagnostic strategies to avoid overtreatment and unnecessary interventions. Early detection techniques, such as ultrasound and Fine-Needle Aspiration Biopsy (FNAB), play a vital role in identifying malignancies at an early stage, enabling timely and appropriate treatment [3].
Non-invasive management strategies, including active surveillance, offer several advantages, particularly for low-risk thyroid cancers. These approaches reduce the need for invasive procedures, minimize surgical complications, and preserve thyroid function, thereby improving patients’ quality of life [4]. However, non-invasive treatments also have limitations, such as the potential for disease progression in a small subset of patients and the psychological burden of living with an untreated malignancy. Therefore, careful patient selection and close monitoring are essential to ensure the safety and effectiveness of non-invasive approaches [5].
Thyroidectomy remains the primary treatment for thyroid malignancies, but it is an invasive procedure associated with potential complications, including recurrent laryngeal nerve injury, hypothyroidism, and hypoparathyroidism, all of which can significantly impact a patient's quality of life [6]. These risks underscore the importance of accurate preoperative diagnosis to minimize unnecessary surgeries and ensure that only patients with confirmed malignancies undergo surgical intervention.
Ultrasound imaging is the cornerstone of the initial diagnostic evaluation for thyroid nodules. It is a non-invasive, widely available, and cost-effective imaging modality that provides detailed information about nodule characteristics, such as size, shape, echogenicity, margins, and vascularity. Ultrasound plays a pivotal role in risk stratification, helping clinicians identify suspicious nodules that require further investigation through FNAB [7]. The use of ultrasound-guided FNAB has further enhanced diagnostic accuracy by ensuring precise sampling of targeted nodules, particularly those that are small or difficult to palpate [8].
Since its introduction in 1981, FNAB has become the gold standard for the preoperative diagnosis of thyroid nodules. It is a rapid, safe, and minimally invasive procedure that has revolutionized the management of thyroid cancer by providing cytological evidence to rule out malignancy [4]. Despite its proven efficacy, FNAB has limitations. Studies report a non-diagnostic rate ranging from 2% to 29%, which can lead to repeated procedures, increased healthcare costs, patient anxiety, and delays in diagnosis. These challenges highlight the need for diagnostic methods that balance high sensitivity and specificity with minimal patient burden and cost [9].
The diagnostic evaluation of thyroid nodules requires a multidisciplinary approach, integrating imaging, cytology, and clinical assessment. Ultrasound serves as the first step in this process, guiding the selection of nodules for FNAB and reducing the likelihood of unnecessary biopsies [10]. However, the limitations of FNAB, particularly its non-diagnostic rate, emphasize the need for complementary diagnostic tools and techniques to improve accuracy and patient outcomes [11].
The ACR TI-RADS system, introduced in 2017, uses a points-based approach to evaluate thyroid nodules based on five sonographic features: composition, echogenicity, shape, margin, and echogenic foci [12]. Nodules are classified into risk levels (TR1 to TR5), with higher levels indicating greater malignancy risk and lower size thresholds for FNA. This system reduces unnecessary biopsies, ensures timely cancer detection, and improves diagnostic consistency [13].
This study aims to compare the accuracy of preoperative (FNAB) and intraoperative (Touch Imprint cytology and Frozen Section Cytology) diagnostic techniques with permanent pathology, the gold standard. By evaluating these methods, we seek to refine the diagnostic pathway for thyroid nodules, reduce non-diagnostic results, and minimize unnecessary surgeries and associated complications. The findings will contribute to improving diagnostic strategies and optimizing patient care in thyroid cancer diagnosis.
2. METHODS
This study was conducted as a retrospective cohort, and 110 individuals were included in the research. The study population consisted of patients with thyroid masses who visited the Shahid Madani Medical Training Center in Karaj and received a clear diagnosis based on final pathology. These patients were recommended for surgical excision of the thyroid mass based on the findings of Fine-Needle Aspiration (FNA), touch imprint, and frozen section tests. Data were collected using the medical record filing system of Shahid Madani Hospital in Karaj for patients who underwent total or partial thyroidectomy between 2014 and 2016.
All patients with a history of thyroidectomy who had complete data required for this study, such as preoperative ultrasound, FNA cytology, and surgical pathology reports, were included. Patients under 15 years old, those with a history of thyroid cancer, individuals who had undergone head and neck radiation, and those who declined to participate in the study for any reason were excluded. Moreover, the following formula was used:
Accuracy: (Sensitivity*prevalence) + (specificity *prevalence -1)
Or (real negative +real positive)/(real negative +real positive +false nagative +false positive)
3. DATA ANALYSIS
The collected data were analyzed using SPSS software version 26. Descriptive statistics were used to summarize the data, and a 95% confidence level was applied. The Chi-square and Spearman tests were used to determine correlations between variables. Sensitivity, specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV), likelihood ratios, and accuracy were calculated and compared for the diagnostic tests [11].
This work was conducted in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
This study was approved by the Research Ethics Board of Alborz University of Medical Sciences (IR.ABZUMS.REC.1399.284).
4. RESULTS
A total of 101 people were assessed to determine who was ill for this reason. The average age of all patients included in the research was 46.34 years, with 74.26% being female and 25.74% being male.
The results of patient ultrasounds and the frequency of TIRADS (Thyroid Imaging Reporting and Data System) subgroups showed that nodules with cysts, nodules with calcification, nodules with calcification and cysts, multinodular goiter, and cysts were the different types of lesions observed.
The TIRADS categories were as follows: TIRADS1, TIRADS2, TIRADS3, TIRADS4, and TIRADS5.
Based on the type of lesion, the frequency of FNA results indicated nodular goiter, papillary carcinoma, follicular adenoma, Hashimoto's thyroiditis, medullary carcinoma, follicular hyperplasia, AUS, Follicular Lesion of Undetermined Significance (FLUS), and lesions suspicious for malignancy.
The outcomes of frozen section and touch imprint cytology were categorized by lesion type, including follicular adenoma, Hashimoto's thyroiditis, medullary carcinoma, lymphoma, thyroglossal cyst, follicular hyperplasia, and nodular goiter.
Permanent pathology outcomes were reported according to the type of lesion, including follicular adenoma, Hashimoto's thyroiditis, medullary carcinoma, follicular carcinoma, lymphoma, anaplastic carcinoma, thyroglossal cyst, follicular hyperplasia, nodular goiter, and papillary carcinoma (Table 1).
| Sonography | |
|---|---|
| Type of lesion | Number (%) |
| Nodule | 24(23.8) |
| Nodule +Cyst | 17(16.8) |
| Nodule + Calcification | 14(13.9) |
| Nodule + Calcification+ Cyst | 22(21.8) |
| Multinodular Goiter | 22(21.8) |
| Cyst | 2(1.9) |
| Total | 101(100) |
| TIRADs | |
| TIRADS | Number (%) |
| TIRADs 1 | 1(0.9) |
| TIRADs 2 | 21(20.8) |
| TIRADs 3 | 34(33.7) |
| TIRADs 4 | 28(27.7) |
| TIRADs 5 | 17(16.8) |
| Total | 101(100) |
| FNA | |
| Type of lesion | |
| Nodular Goiter | 32(31.7) |
| Papillary Thyroid Carcinoma | 25(24.8) |
| Follicular adenoma | 2(1.9) |
| Hashimoto's thyroiditis | 1(0.9) |
| Medullary carcinoma | 3(2.8) |
| Follicular Carcinoma | 7(6.9) |
| AUS | 9(8.9) |
| FLUS | 2(1.9) |
| Suspected of malignancy | 10(9.9) |
| Follicular neoplasia | 1(0.9) |
| Benign tumor | 9(8.9) |
| Total | 101(100) |
| Permanent pathology | |
| Type of lesion | |
| Nodular Goiter | 44(44.57) |
| Papillary Thyroid Carcinoma | 28(27.7) |
| Follicular adenoma | 7(6.9) |
| Hashimoto's thyroiditis | 6(5.9) |
| Medullary carcinoma | 3(2.9) |
| Follicular Carcinoma | 4(3.9) |
| Lymphoma | 2(1.9) |
| Anaplasia carcinoma | 2(1.9) |
| Thyroglossal cyst | 2(1.93) |
| Follicular hyperplasia | 2(1.9) |
| Total | 101(100) |
| Frozen Section | |
| Type of lesion | |
| Nodular Goiter | 59(58.35) |
| Papillary Thyroid Carcinoma | 24(23.8) |
| Follicular adenoma | 1(0.9) |
| Hashimoto's thyroiditis | 4(3.9) |
| Medullary carcinoma | 4(3.9) |
| Lymphoma | 2(1.9) |
| Thyroglossal cyst | 2(1.95) |
| Follicular hyperplasia | 5(4.9) |
| Total | 101(100) |
| Touch imprint cytology | |
| Type of lesion | |
| Nodular Goiter | 59(57.35)valid |
| Papillary Thyroid Carcinoma | 24(22.8) |
| Follicular adenoma | 2(1.9) |
| Hashimoto's thyroiditis | 4(3.9) |
| Medullary carcinoma | 5(4.9) |
| Lymphoma | 2(1.9) |
| Thyroglossal cyst | 2(1.95) |
| Follicular hyperplasia | 5(4.9) |
| Total | 101(100) |
Table 2 explains the diagnostic FNA, touch imprint, and frozen section tests. According to the results of permanent pathology, there were 39 cases of thyroid cancer, compared to the 28, 29, and 30 cases of cancer reported by FNAB, touch imprint, and frozen section cytology, respectively. Compared to permanent pathology, the accuracy of FNAB, touch imprint, and frozen section cytology in predicting cancer risk was 87.12%, 89.1%, and 91.09%, respectively.
Figs. (1 and 2) demonstrate that all three diagnostic techniques are highly accurate in detecting thyroid cancer, albeit frozen section cytology is superior to the others when evaluated individually.
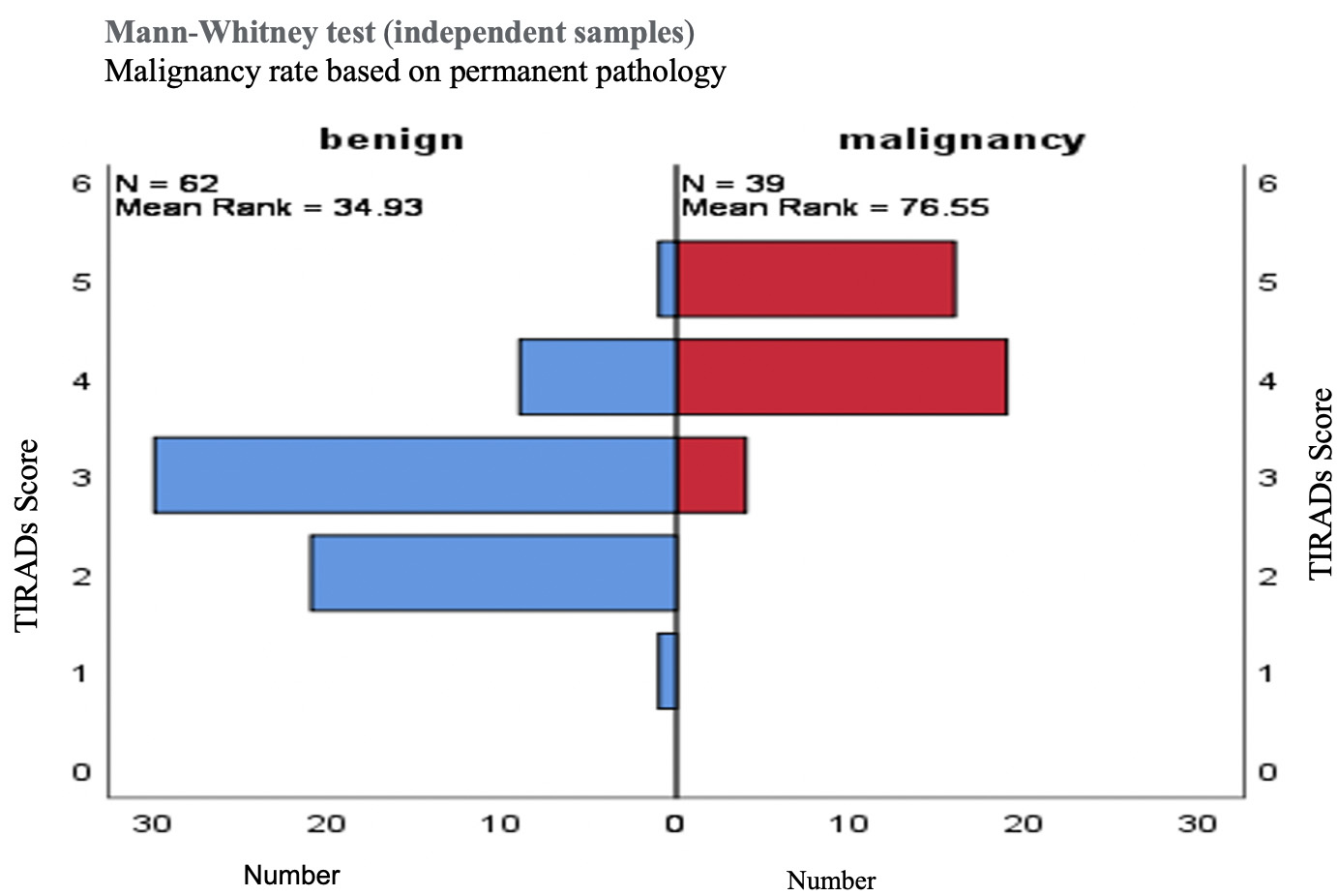
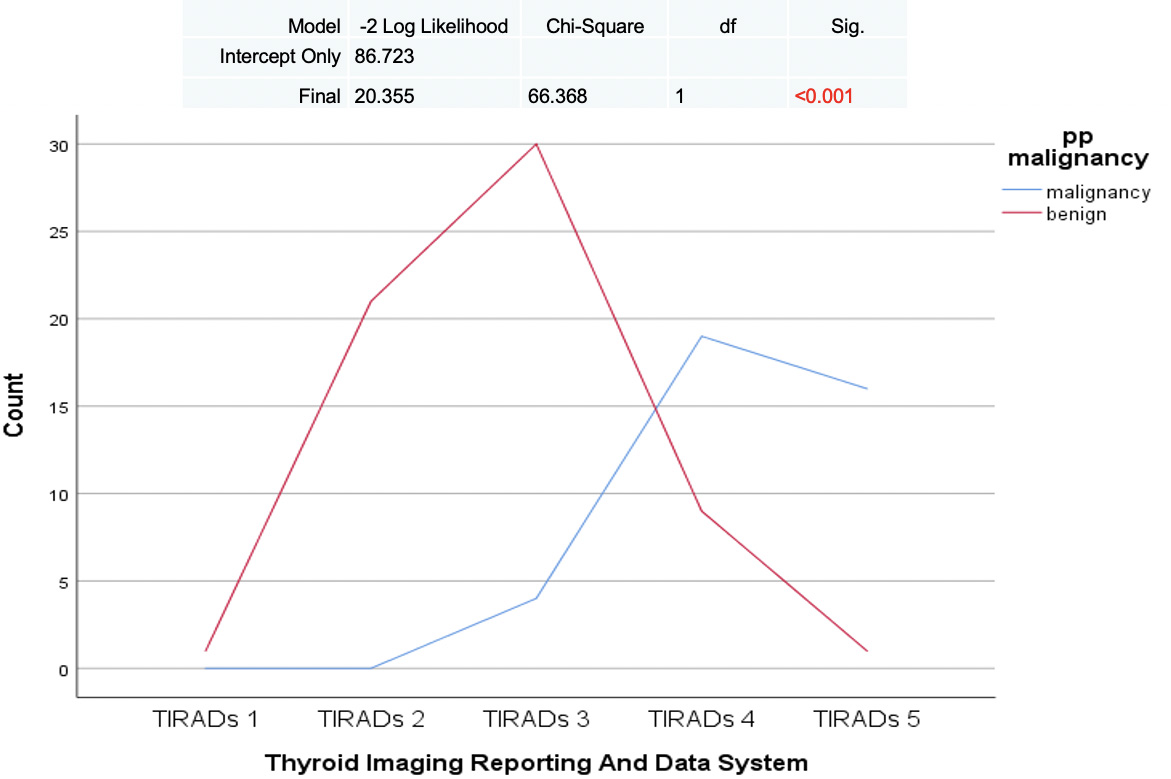
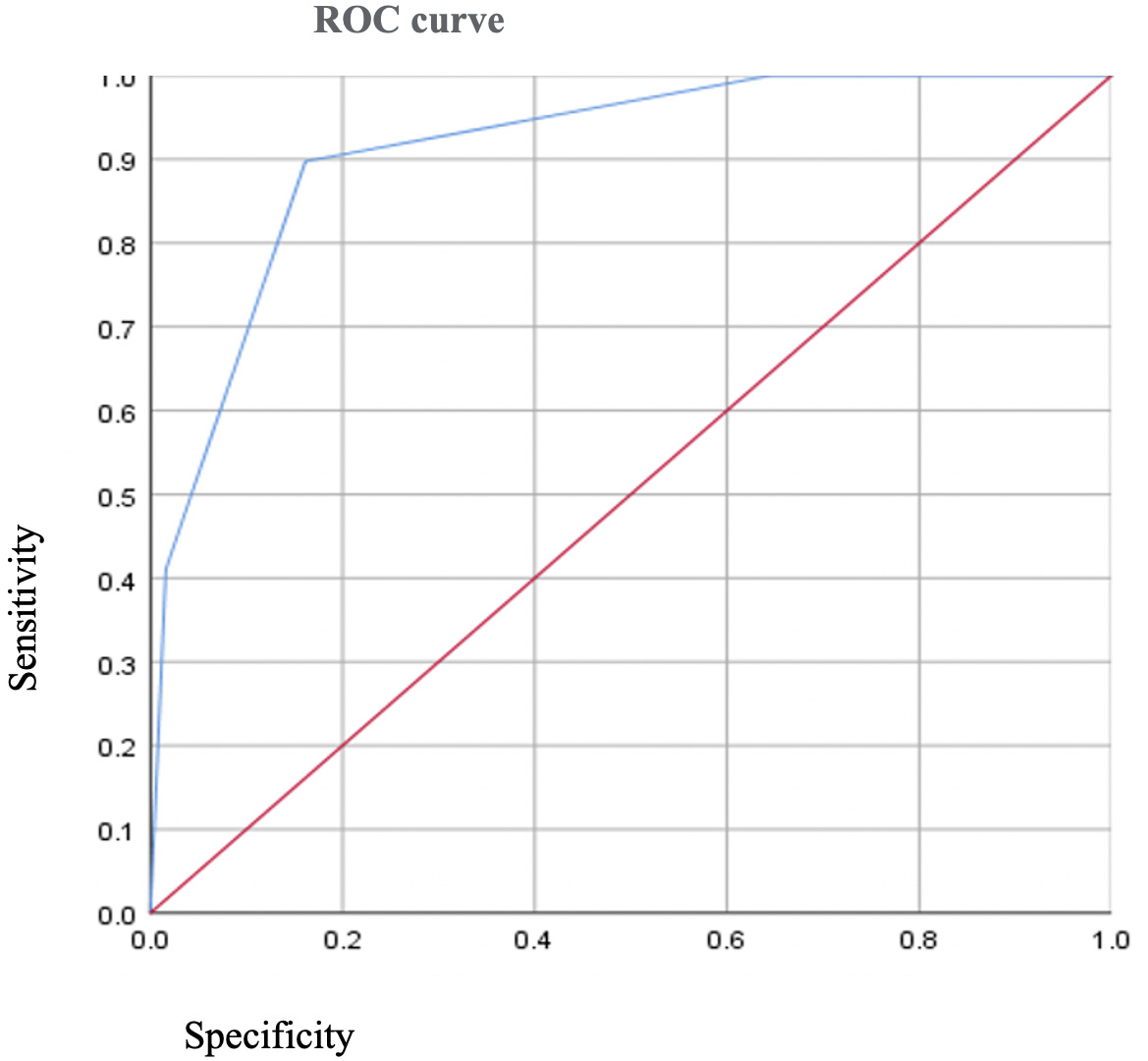
It can be concluded that the reported value of TIRADS > 3 was effective in ruling out the malignancy. The Thyroid Imaging Reporting and Data System (TIRAD) of malignancy (Fig. 3) can be claimed based on the findings of the probability ratios, which are as follows:
Sensitivity: 91.2%, Specificity: 83%, PPV: 77.14, NPN: 93.76, Accuracy: 86%, Positive alignment: 5.35, and negative alignment: 0.1 (Fig. 3).
These results highlight the effectiveness of the diagnostic approach in distinguishing between benign and malignant thyroid nodules.
| FNAB | |||||
|---|---|---|---|---|---|
| Malignant | Permanent Pathology | Malignant | Benign | Confidence Interval | |
| Number | 27 | 1 | - | ||
| Sensitivity | 69.2% | 82.2%-53.8% | |||
| PPV | 96.4% | 99.8%-85.2% | |||
| Benign | Number | 12 | 61 | - | |
| Specificity | 98.4% | 99.9%-93.1% | |||
| NPV | 83.6% | 90.8%-74% | |||
|
Touch imprint |
|||||
| Malignant | Number | 29 | 1 | - | |
| Sensitivity | 74.4% | - | 86.2%-59.4% | ||
| PPV | 96.7% | - | 99.8%-86.1% | ||
| Benign | Number | 10 | 61 | - | |
| Specificity | 98.4% | 99.9%-93.1% | |||
| NPV | 85.9% | 92.7%-76.6% | |||
| Frozen Section | |||||
| Malignant | Number | 30 | 0 | - | |
| Sensitivity | 76.9% | - | 60.67-88.87% | ||
| PPV | 100% | - | - | ||
| Benign | Number | 9 | 62 | - | |
| Specificity | 100% | - | 94.22-100% | ||
| NPV | 87.33% | - | 79.53-92.44% | ||
NPV = Predictive Value Negative
Positive and negative validity test: (FNA: 42.9 - 0.313), (Touch imprint: 46.10- 0.26), Frozen Section (50-0.23).
5. DISCUSSION
While physical examination, scintigraphy, and ultrasound offer initial insights into thyroid nodules, they cannot reliably differentiate benign from malignant nodules. Preoperative FNA biopsy and intraoperative techniques like Frozen Section (FS) and cytological methods(touch-imprint and crush preparation) are essential for accurate diagnosis and management, which are now routinely used in practice [7, 8, 14].
FNA is the most accurate and cost-effective preoperative tool, with over 80% diagnostic accuracy [5, 13, 7]. However, it has limitations in non-diagnostic cases and follicular lesions, prompting intraoperative FS to improve malignancy detection [9, 15, 16].
Touch-imprint cytology, valued for its cellular richness, is preferred by pathologists but has limitations in detecting vascular and capsular invasion. Thyroid nodules are common, and diagnostic methods like FNA, touch-imprint, and crush preparation are widely used for evaluation [14].
It should be noted that intraoperative cytology methods are more sensitive than those that have FNA to diagnose thyroid malignancies. The findings of this study are consistent with the findings of earlier studies in this field and demonstrate that all three of these methods have very high accuracy for detecting malignancy in thyroid nodules [17].
The sensitivity, specificity, and accuracy of the intraoperative procedures vary somewhat, and these variations show a small preference for the frozen section approach over touch imprint cytology [18].
Chehrei et al. concluded in a 2012 article that the frozen section technique had a 100% sensitivity, specificity, and accuracy rate compared to the 78.6%, 95%, and 92.4% rates of the touch imprint method, respectively [19]. They calculated these indicators for the combined use of touch imprint and frozen section methods and reported the results in the following order: 100%, 97.6%, and 98.18% before concluding that intraoperative cytology techniques like touch imprint and frozen section are relatively inexpensive and practical methods for accurate diagnosis and can minimize the number of unnecessary surgeries. When these techniques are used together, the accuracy rate is also increased to 98.1% and 97.6%.
The findings were the same as those from another study conducted by Ahmadinejad et al. in 2015 to assess the sensitivity, specificity, and positive and negative predictive values of FNAB, touch imprint cytology, and crash preparation compared to permanent pathology [20]. The sensitivity, specificity, and positive and negative predictive values were 95.3%, respectively, for the FNAB approach. The same indicators were observed completely similarly and even better in the remaining two tests, scoring 80%, 100%, 100%, and 96.7%. This study concluded that crash preparation, touch imprint cytology, and FNAB all had adequate diagnostic value when compared to permanent pathology.
To test the sensitivity and specificity of FNAB in 2004, Gharib et al. examined 19,520 samples. They eventually concluded that if FNAB reports a case as benign, the probability of malignancy is 1%, and if it reports a case as suspicious and malignant, the probabilities of malignancy are 20% and 100%, respectively [21].
To determine the sensitivity and specificity of FNA for the diagnosis of cancer in thyroid nodules, Kuru et al. studied 662 individuals in 2010 [21]. They concluded that FNA has a sensitivity of 65-98% and a specificity of 72-100%. However, one research claims that nodules larger than 4 cm have a greater rate of false negative results for this test [22].
Therefore, based on the research and our investigation, it is conceivable to employ diagnostic techniques within the operating room to determine the kind of thyroid masses and select the appropriate surgical approach or avoid unnecessary operations.
Given the limited number of samples in this study and the insufficient data regarding the accuracy of ultrasound, it is recommended that further studies with larger sample sizes be conducted. These studies should investigate the relationship between reported TIRADS scores and malignancies, with variables, such as age, gender, BMI, the type of ultrasound device used, the type and size of the probe, and the radiologist's level of experience. This approach could help utilize a simple, cost-effective, and accessible diagnostic method, thereby reducing the unnecessary use of invasive tests and the additional financial burden imposed on the public and the healthcare system.
CONCLUSION
According to the study's findings, FNAB, touch imprint, and frozen section cytology are very accurate in identifying thyroid cancers when compared to permanent pathology. Therefore, they may be used as a trustworthy alternative to invasive and costly techniques like surgery for the diagnosis of thyroid cancers.
AUTHORS’ CONTRIBUTIONS
Dr. Yasmina Ahmadinejad and Dr. Mohammad Saeed Kahrizi: conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. Dr. Mojtaba Ahmadinejad and Dr. Izadmehr Ahmadinejad: Designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript. Dr. Ali Soltanian and Dr. Kimia Ghanbari Mardasi: Coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content.
LIST OF ABBREVIATIONS
| FNAB | = Fine-Needle Aspiration Biopsy |
| FNA | = FineNeedle Aspiration |
| PPV | = Positive Predictive Value |
| NPV | = Negative Predictive Value |
| FLUS | = Follicular Lesion of Undetermined Significance |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Research Ethics Board of Alborz University of Medical Sciences, Iran (IR.ABZUMS.REC.1399.284).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
Declared none.


